CPT 15271: Under Skin Substitute Grafts Guide

CPT 15271: Under Skin Substitute Grafts Guide
When it comes to wound care and complex skin injuries, accurate coding is just as important as the treatment itself. One commonly reported code in wound management is CPT 15271 – Under Skin Substitute Grafts.
For healthcare providers across the United States, understanding how to bill this code correctly can directly impact reimbursement, compliance, and overall healthcare revenue cycle management. In this guide, we’ll break down what CPT 15271 covers, when it should be used, and how professional medical billing services can help avoid costly errors.
What is CPT 15271?
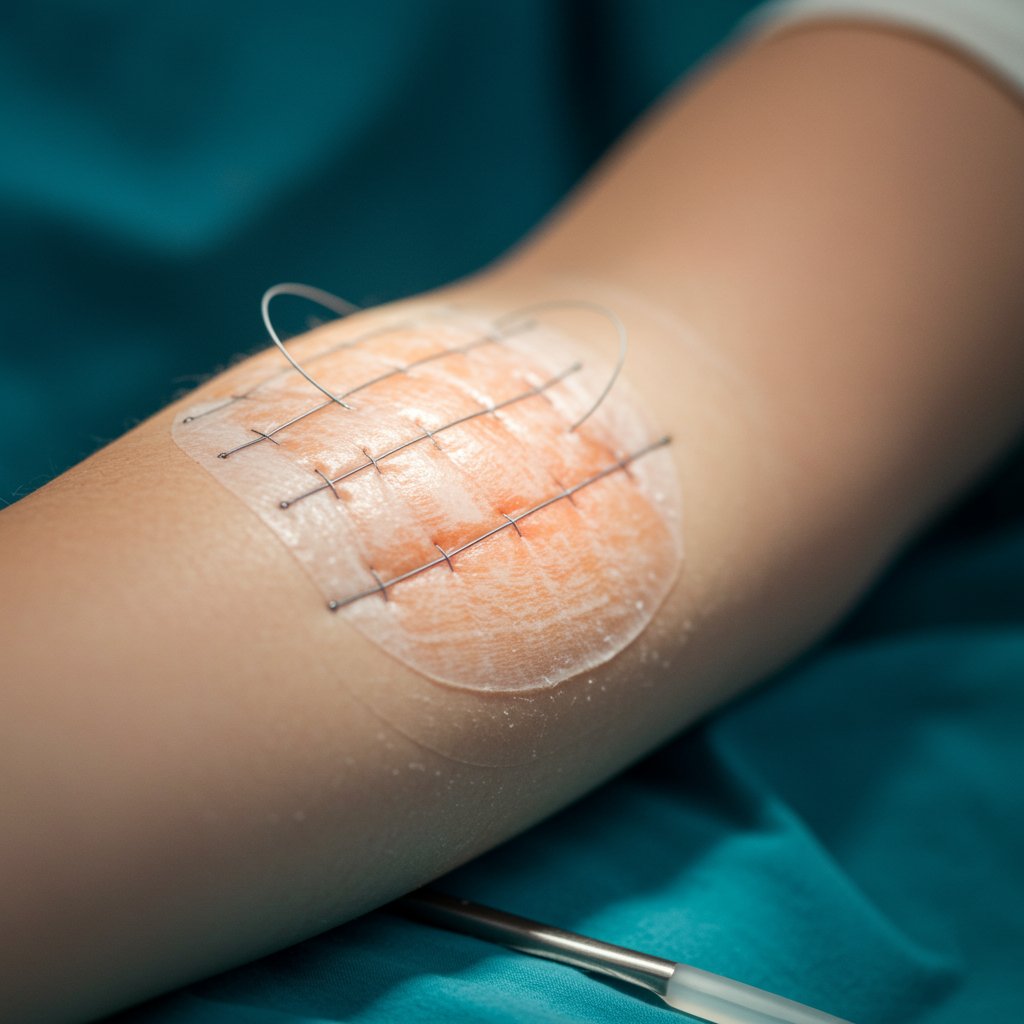
CPT 15271 is used for the application of a skin substitute graft to a wound. It typically applies to the initial application of a skin substitute to areas such as:
The trunk
Arms
Legs
This code is often reported in cases involving:
Chronic non-healing wounds
Diabetic ulcers
Venous stasis ulcers
Traumatic wounds
Post-surgical wound complications
Skin substitute grafts are bioengineered or biologically derived materials applied over wounds to promote healing and tissue regeneration.
When Should CPT 15271 Be Used?
CPT 15271 is reported for the first 25 sq cm or less of wound surface area. If the treated area exceeds 25 sq cm, add-on codes may apply for each additional 25 sq cm.
It is important to note:
Documentation must clearly state wound size.
The product used must be identified.
The medical necessity of the graft must be supported.
Prior treatments and failed conservative therapies should be documented.
Proper documentation plays a key role in successful reimbursement. Even a small error can result in denials or delayed payments.
Key Documentation Requirements
To ensure proper reimbursement under healthcare revenue cycle management protocols, providers should include:
Detailed wound description (size, depth, location)
Date of service
Product name and type of skin substitute
Application technique
Medical necessity
Progress notes and treatment plan
A skilled medical billing specialist reviews these details carefully before submission to reduce claim denials.
Common Billing Challenges with CPT 15271
While the procedure may seem straightforward, billing for skin substitute grafts can get complex. Common issues include:
Incorrect surface area calculation
Missing product documentation
Improper modifier usage
Confusion between graft placement vs. simple wound care
Payer-specific coverage policies
Many practices lose revenue because claims are either undercoded or denied due to insufficient documentation.
This is where experienced medical billing and coding services make a difference. Having certified coders review claims before submission can protect your practice from revenue leakage.
The Role of RCM Services in Wound Care Billing
Managing claims for advanced wound care procedures like CPT 15271 requires strong rcm services processes.
A streamlined system includes:
Insurance eligibility verification
Prior authorization support
Accurate charge capture
Timely claims submission
Denial management
Appeals processing
A reliable medical billing company ensures that each step is handled carefully so providers can focus on patient care instead of paperwork.
Importance of Accurate Medical Coding
Skin substitute grafts may involve product costs, supply billing, and facility charges depending on the setting. Errors in medical coding services can lead to compliance risks or financial setbacks.
Accurate coding ensures:
Proper reimbursement
Reduced audit risk
Improved cash flow
Regulatory compliance
Credentialing also plays a major role here. If providers are not properly enrolled with payers, even correctly coded procedures may face payment delays.
How Theiatrics Supports Providers in the USA
For healthcare providers looking to simplify complex billing processes, Theiatrics offers end-to-end medical billing services designed specifically for U.S. practices.
From coding CPT 15271 accurately to managing full healthcare revenue cycle management workflows, Theiatrics supports:
Specialty practices
Wound care clinics
Ambulatory surgery centers
Physician groups
Their trained medical billing specialist team ensures:
Clean claims submission
Reduced denial rates
Compliance with payer policies
Transparent reporting
If your facility struggles with recurring denials or delayed payments for advanced procedures like under skin substitute grafts, it may be time to optimize your billing strategy. You can always contact us to learn more about customized solutions for your practice.
Why Outsourcing Medical Billing Makes Sense
Handling wound care billing internally can strain staff resources. Outsourcing to a professional medical billing company offers:
Lower administrative burden
Access to experienced coding professionals
Faster claim turnaround
Better cash flow visibility
Scalability as your practice grows
When combined with professional medical coding services, outsourcing creates a strong financial backbone for your clinic.
Final Thoughts
CPT 15271 plays an important role in wound care reimbursement. However, its complexity makes accuracy critical. From documentation to surface area calculation and payer compliance, each detail matters.
With expert support in medical billing and coding services, healthcare providers can reduce denials and strengthen their healthcare revenue cycle management processes.
If your practice is looking to improve efficiency, reduce errors, and maximize reimbursements for under skin substitute graft procedures, partnering with an experienced RCM partner like Theiatrics can make a measurable difference
Get The Free Consultation Service
© 2024 Theiatrics. All Rights Reserved